I posted on the Facebook page for this blog recently about a visit I made to a nutritionist. I had won, at an auction for the SSF (or rather, my husband won for me), a one hour consult with Tara Mardigan, MS, MPH, RD. She is a nutritionist in Boston, MA and also serves on the Sjögren’s Syndrome Foundation’s Medical and Scientific Advisory Board. Some of my readers asked if I would post the information about that visit and this is what today’s entry is all about.
Anybody who follows my blog know that I feel very strongly that diet and nutrition play a huge part in dealing with autoimmune illnesses and is a very underutilized treatment option for all patients. I was running into a few issues with my nutrition lately, mostly because I was freaking out over what I was “supposed” to do. Since my diagnosis, I have been vegetarian, gluten and dairy-free, Paleo, and on the Autoimmune Protocol. I have had significant relief at times with the gluten and dairy-free, as well as the Paleo. However Paleo was causing me some other problems physically, so I had to loosen up on that. The Autoimmune Protocol didn’t seem to do me much good except make it so that I became a recluse in my house because I couldn’t eat anywhere else.
I have some emotional issues around food as well, many of which have improved over the past few years, but still come back to haunt me when my stress level is high. This most notably happens when I am stressed out over medical issues. I definitely have an addiction issue around sugar, processed foods, fast foods, etc. So going in all these different directions with my diet was really just making these issues worse over the past six months. I wanted to eat to fuel and heal my body, but it felt like the more restrictions I imposed on myself, the worse my eating habits would get after a while.
I was curious to see what an actual nutritionist had to say about it all, so off to Boston I went. Honestly, I am in Boston so much, I should just move there! The visit went well and the following is the recommendations she made to me in regards to my diet. Please remember, these suggestions are for me; most likely, you will have different needs so these suggestions should not be considered appropriate for everyone. That being said, I think a lot of the suggestions are just a good way to eat for all of us:
* Aim for a bigger, more balanced breakfast.
* Aim for balance at mealtime using the Five Fingers Chart. This chart states that at every meal, you should strive to eat one serving from each of the following groups: fruit/vegetable; carbohydrate, protein, healthy fat, and fluid. You can eat more than one serving of vegetables/fruits (except for starchy veggies and dried fruit). The more color, the better. Choose smaller portions for tropical fruits.
* Aim for a Powerful Plate at dinnertime. Choose the Healthy Eating Plate on days you exercise (50% vegetables/fruits, 25% carbohydrates, 25% protein) and the Less Active Plate on days you don’t exercise or have a very light day (75% vegetables/fruits, 25% protein). Adjust the amount of carbohydrates you take in based on your activity level. Less active, less carbs.
* Count corn, winter squash, parsnips, peas, and potatoes as carbohydrates, not as vegetables.
* Fruit with skin: 1 medium-large piece or 1 cup (berries, apples, pears, grapes, plums, nectarines,oranges, grapefruit.
* Fruit without skin: 1 small banana or 1/2 up (any tropical fruit)
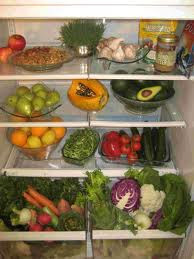
* Consider a high powered blender such as Vitamix or Blendtec to support your efforts and increasing fruits and vegetables (significantly) in smoothies will be a great anti-inflammatory nutrition strategy.
*Try adding an intentional healthy snack between breakfast and lunch and/or lunch and dinner if you have a gap of more than 3-4 hours between. Fruit with 0.25 cup of nuts or unsalted pumpkin seeds or sunflower seeds is a great choice here. You are looking for fiber, a small amount of healthy fat and/or protein.
*Consider trying some non-gluten free options from fresh-made sources. Refer to FODMAP grocery list for some digestive-friendly choices (not necessarily gluten-free).
* Try fresh cut vegetables, such as cucumbers or carrots with red wine or white vinegar as a crunchy nighttime snack that’s sodium-free and low in calories.
* Consider the “One Bowl” method for nighttime or mindless snacking. You can eat whatever you want (healthy or unhealthy) but you’ll first stop and put the food into a bowl. Don’t judge the food or the amount, but take a minute to pause. This is a mindful eating strategy and may help you gradually make intentional choices that help nourish. This is a difficult strategy but if you’re able to stick with it, it will help you lose weight because you’ll eat less and choose more healthful options. The book that inspired this idea is One Bowl by Don Gerrard.
* Be verbal when eating out. Ask for extra vegetables, prepared without butter or sauces. Ask for a side of pasta or skip it. Skip the bread. Avoid shiny and battered foods. Get open-faced sandwiches. Have the burrito bowl with a small spoonful of rice. Skip or split appetizers and desserts. Choose fish instead of meat. Ask for lemon wedges to add flavor.
* When dressing your salad, use fresh lemons and a small amount of olive oil. If you want creamy dressing, ask for it on the side and use a small amount.
* Continue with consistent (but gradual) hydration throughout the day with water.
* Great job with exercise. Continue with walking and yoga and hopefully you will be able to gradually get back into running again.
Whew! I know that’s a lot of information, but I thought it was important enough to share with all of you. I had the appointment right before Christmas. I did read the One Bowl book she mentioned and started to implement a few of the suggestions, but Christmas eating really threw me off. I did try some non-GMO bread with gluten in it. I found that in small amounts (and I mean SMALL), I could tolerate it, but larger amounts seem to be a problem. I found this out when I dropped my gluten and dairy restriction for several weeks around Christmas. I also developed a lot of digestive issues when I ate a lot of gluten and dairy, issues that I have never had before. I am currently on the last day of a 10 day detox/cleanse which was my own doing; it was NOT a recommendation of the nutritionist. I will be blogging about that tomorrow or Monday. My plan for the few days following the detox is to ease back into eating normally again and then go full steam ahead with the nutritionist’s suggestions.
One of the big things that this visit made me realize and understand is that despite all the different “diets” and eating plans out there that claim to cure or help your autoimmune illness, in the end, it may just come down to great nutrition on a consistent basis for many people. I am not saying that the Autoimmune Protocol or eliminating gluten may not help your symptoms; I know many people who find relief eliminating different food groups, such as with me and gluten. However, I think that for me, the answer may be more in eating whole foods in balance with each other, minus the gluten and dairy I need to limit, as well as limiting processed foods, soy, alcohol, refined sugar, etc. So basically, just eating healthy!
Please feel free to comment below on what nutrition strategies you have implemented to help your autoimmune illness, or even just your general health.